Understanding Type 1 Diabetes: What You Need to Know
Diabetes type 1 is a chronic illness also referred to as juvenile diabetes or insulin-dependent diabetes. The pancreas produces little or no insulin in this situation. The hormone insulin is what the body uses to let glucose, or sugar, into cells so those cells can make energy. Type 1 diabetes can be brought on by a number of variables, including some viruses and genetics. Type 1 diabetes can strike adults even though it typically first manifests in childhood or adolescence. There is still no cure for type 1 diabetes, despite much research. In order to avoid problems, treatment focuses on controlling blood sugar levels using insulin, food, and lifestyle changes.
Symptoms of these DiabetesThe main symptoms of type 1 diabetes develop over a short period of time, usually weeks or months, and include: increased thirst, frequent urination, hunger, weight loss despite increased appetite, fatigue, irritability, blurred vision, and fruity-smelling breath. These occur as a result of high blood glucose levels as the body cannot properly regulate its blood sugar levels without insulin. Someone with these diabetes will need to inject insulin or use an insulin pump on a daily basis for the rest of their life.
 |
| Type 1 Diabetes |
Causes and Risk Factors
Unlike type 2 diabetes, Type 1 Diabetes is not caused by lifestyle or environmental factors. It is an autoimmune disease where the body's own immune system destroys the insulin-producing cells in the pancreas in a misguided attack. Researchers believe genetics play a role in susceptibility, but the exact causes are still unknown. Those at higher risk include those with a family history of diabetes or other autoimmune diseases like thyroid disease. Viruses have also been linked as potential triggers that may stimulate the autoimmune response in genetically predisposed individuals.
Testing and Diagnosis
These diabetes is diagnosed through a simple blood test that checks for high blood glucose levels, both randomly as well as after fasting. Low levels of insulin in the blood and the presence of diabetes autoantibodies also suggest type 1 diabetes. A doctor may also request an HbA1c test which measures average blood glucose levels over 2-3 months, with levels of 6.5% or above indicating diabetes. Diagnosis is usually confirmed by an oral glucose tolerance test which checks how the body processes sugar over a period of time.
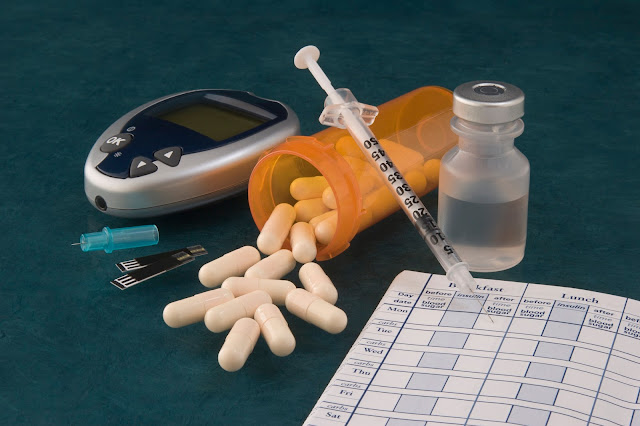
Treatment with Insulin Therapy
As type 1 diabetes is caused by a lack of insulin production, daily insulin injections or continuous insulin administration through an insulin pump are vital for treatment. Multiple daily injections or continuous infusion aim to closely match natural insulin secretion and keep blood glucose levels in a target range. Individualized meal plans along with blood glucose monitoring several times a day help determine appropriate insulin dosing. Education on effective insulin management strategies is also important. Other aspects of care like nutrition, exercise, and avoiding health risks complete a comprehensive diabetes management plan.
Potential Complications If Untreated
Without proper management and insulin treatment, extremely high or fluctuating blood glucose levels associated with uncontrolled type 1 diabetes can lead to devastating complications. In the short-term, ketoacidosis may develop due to lack of insulin, potentially resulting in diabetic coma. Over many years, high blood glucose causes damage to blood vessels and nerves throughout the body. Common long-term complications include: kidney disease, eye disease causing vision loss, nerve damage (diabetic neuropathy), foot problems that may require amputation, skin conditions, hearing impairment and heart disease. Good control through diligent self-care and medical supervision is therefore vital to reducing risk.
The Challenge of Balancing Life with Diabetes
Managing type 1 diabetes involves a daily balancing act of lifestyle factors and medication that is challenging emotionally and practically. Around-the-clock glucose monitoring, multiple insulin injections or use of an insulin pump, meticulous counting of carbohydrates, physical activity and dealing with hypo- and hyperglycemic episodes take a considerable ongoing effort. This places immense responsibilities on not just individuals with diabetes but also caregivers and families. The fear of hypoglycemia, the frustration of fluctuating blood sugars despite efforts, as well as the need for lifestyle adjustments adds considerable psychological stress. Support groups and mental health support help empower people to successfully adapt while maintaining healthy coping mechanisms.
Advances in Treatment and Management
Significant research is underway to better understand the autoimmune causes of this diabetes and find disease-modifying or preventive therapies to preserve endogenous insulin production. Stem cell transplants show promise in restoring insulin secretion. Advances in insulin formulations, glucose monitoring technology and insulin delivery devices seek to make management increasingly convenient and mimic natural patterns.
There is hope that artificial pancreas systems combining automated insulin delivery and glucose sensing may someday provide an "open-loop" system to remove much of the intensive manual effort for people with type 1 diabetes. Overall, while a cure still remains elusive, modern management strategies together with individualized care plans have vastly improved quality of life and reduced risks of complications for those living with this diabetes. With continued research and support, living well with this condition can remain very achievable.


Comments
Post a Comment